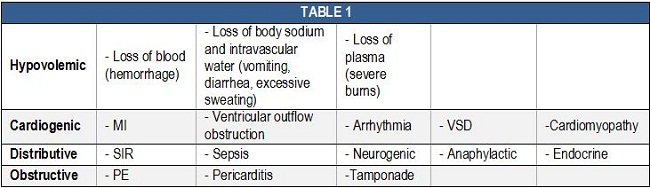
Things were much simpler back in the Roman days. When one was stabbed by a sword he/she bled and died of “cold” — or hypovolemic — shock. If the person got lucky and was only wounded by the dirty blade, they probably died of “warm” — or septic — shock. Today our knowledge has advanced well past “cold” and “warm,” and leaves us with at least 10 types of shock commonly encountered in the emergency department (ED) and intensive care unit (ICU) (Table 1). Each represents a constellation of physiologic effects that require a tailored approach to management. Cardiovascular support with the assistance of vasopressors is a common method, while identification and treatment of the underlying disease process remains the ultimate goal.1
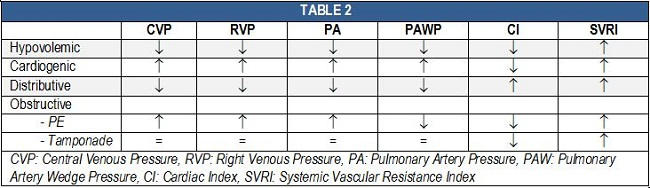
Simply put, shock is inadequate end-organ perfusion. When approaching a patient in shock, one must be aware of the various parameters that may aid in the definitive diagnosis (Table 2), while other hints, such as patient presentation and lab values, will be of initial benefit. Therefore, we cannot completely discard the principles of “cold” and “warm,” but may rather use them as primary markers and then focus on the ABGs, lactic acid, urine output, invasive pressure monitoring and all those other modern tools we now have available. While pulmonary artery catheterization was popular in the past, recent trends show a decline since studies have failed to show a benefit from its routine use.2-4
Institutional shock protocols may vary slightly, and therefore, a definitive guide to the pharmacological selection process may not apply here. However, a list of commonly used vasoactive medications is presented in Table 3, and it is not uncommon to see a multitude of these agents used at the same time as we try to balance out the body’s response to shock, and assist it in its ultimate goal of survival. It is also of note that the selection of the initial agent may simply be based on the patient’s current cardiovascular status, i.e. heart rate and/or blood pressure, with subsequent agents added as needed. What about fluid resuscitation? Generally speaking, we have to “fill the tank” before applying vasopressors. This is particularly important for hypovolemic and distributive shock, but may be tricky in cardiogenic shock due to the potential for pulmonary edema. Clinical judgment will guide you in selecting the proper volume of fluid resuscitation in shock and recognizing when a fluid overload state has been reached (listen to those lung sounds!).
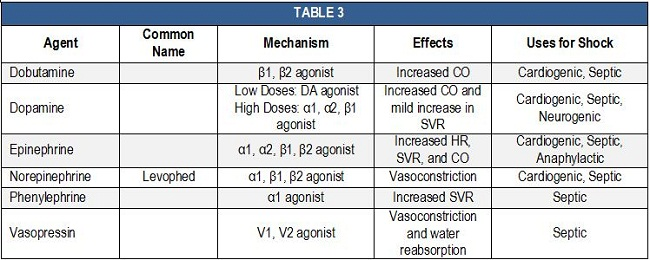
Table 3. http://circ.ahajournals.org/content/118/10/1047.full
References
1. Shoemaker WC. Temporal physiologic patterns of shock and circulatory dysfunction based on early descriptions by invasive and noninvasive monitoring. New Horiz. 1996; 4:300.
2. Connors AF Jr, Speroff T, Dawson NV, et al. The effectiveness of right heart catheterization in the initial care of critically ill patients. SUPPORT Investigators. JAMA. 1996; 276:889.
3. Harvey S, Harrison DA, Singer M, et al. Assessment of the clinical effectiveness of pulmonary artery catheters in management of patients in intensive care (PAC-Man): a randomised controlled trial. Lancet. 2005; 366:472.
4. Shah MR, Hasselblad V, Stevenson LW, et al. Impact of the pulmonary artery catheter in critically ill patients: meta-analysis of randomized clinical trials. JAMA. 2005; 294:1664.
5. http://circ.ahajournals.org/content/118/10/1047.full
Author: Alexander A. Simakov, MPH FP-C MSIV, Medical Student Council, International Ex Officio Representative
